Scleroderma is a complex and often debilitating autoimmune condition that affects millions of individuals worldwide. While the search for a cure continues, recent advancements in medical research and treatment options have provided renewed hope for those living with this challenging disorder. In this comprehensive guide, we’ll explore the latest developments in scleroderma management, delving into the potential for reversing or effectively managing the symptoms of this condition.
Scleroderma, also known as systemic sclerosis, is a chronic and progressive disease that affects the connective tissues of the body, leading to the hardening and thickening of the skin and internal organs. This condition can be incredibly challenging to live with, as it often leads to a wide range of debilitating symptoms, from joint pain and skin tightness to organ dysfunction and life-threatening complications.
However, the landscape of scleroderma treatment is rapidly evolving, with researchers and healthcare professionals working tirelessly to develop new and more effective therapies. This guide will delve into the latest advancements in conventional treatments, as well as explore the potential of emerging approaches, including lifestyle modifications, dietary interventions, and alternative therapies. By understanding the latest treatment options and management strategies, individuals with scleroderma can take an active role in their care and potentially achieve better outcomes.
Key Takeaways
- Scleroderma is a complex autoimmune disorder that affects the connective tissues of the body.
- Recent advancements in medical research have provided renewed hope for those living with scleroderma.
- This guide explores the latest developments in scleroderma management, including conventional treatments, lifestyle modifications, and emerging therapies.
- Individuals with scleroderma can take an active role in their care by understanding the latest treatment options and management strategies.
- With the right approach, it may be possible to effectively manage or even reverse the symptoms of scleroderma.
Understanding Scleroderma: An Overview
Scleroderma, also known as systemic sclerosis, is a complex autoimmune disease that affects the connective tissues in the body. It is characterized by the hardening and thickening of the skin, as well as the potential involvement of internal organs. Scleroderma is a challenging condition, but understanding its nature and various forms can pave the way for effective scleroderma management and, in some cases, the possibility of autoimmune disease reversal.
What is Scleroderma?
Scleroderma is a chronic, progressive disease that causes the overproduction of collagen, leading to the hardening and tightening of the skin and connective tissues. This abnormal process can also affect the internal organs, such as the lungs, heart, and kidneys, making scleroderma a systemic condition. The exact cause of scleroderma is not fully understood, but it is believed to involve a combination of genetic and environmental factors that trigger an autoimmune response.
Types of Scleroderma
There are two main types of scleroderma:
- Localized scleroderma, which affects limited areas of the skin, such as the face, hands, or limbs.
- Systemic scleroderma, which can involve the skin as well as the internal organs, leading to more widespread and potentially life-threatening complications.
Common Symptoms
The symptoms of scleroderma can vary widely, depending on the type and severity of the condition. Some of the most common symptoms include:
- Skin tightening and hardening
- Raynaud’s phenomenon (a condition that causes the fingers and toes to turn white, blue, or red in response to cold or stress)
- Digestive issues, such as heartburn, difficulty swallowing, and constipation
- Lung and heart problems, including pulmonary hypertension and heart rhythm abnormalities
- Joint and muscle pain, as well as limited range of motion
Understanding the various aspects of scleroderma is crucial for developing effective scleroderma management strategies and exploring the potential for autoimmune disease reversal.
The Science Behind Scleroderma
Scleroderma, an autoimmune disease, is a complex condition with intricate underlying mechanisms. To better understand this disorder and explore potential treatment options, including autoimmune disease reversal, it is crucial to delve into the science behind scleroderma.
Immune System Dysfunction
At the heart of scleroderma lies an immune system malfunction. In this condition, the immune system mistakenly attacks the body’s own healthy tissues, leading to excessive collagen production and the hardening of the skin and internal organs. This autoimmune response is a key driver of scleroderma’s progression and the associated debilitating symptoms.
Genetic Factors
Genetic predisposition plays a significant role in the development of scleroderma. Certain genetic variations and mutations have been linked to an increased risk of the disease. While the exact genetic mechanisms are not fully understood, ongoing research is exploring the genetic factors that contribute to scleroderma and the potential for targeted scleroderma treatment.
Environmental Triggers
Environmental factors, such as exposure to certain chemicals, toxins, or infections, may also contribute to the onset of scleroderma. These environmental triggers can interact with genetic predispositions, resulting in the activation of the autoimmune response and the progression of the disease. Understanding the interplay between genetic and environmental factors is crucial for developing effective autoimmune disease reversal strategies.
| Immune System Dysfunction | Genetic Factors | Environmental Triggers |
|---|---|---|
| Autoimmune response leading to excessive collagen production and tissue hardening | Genetic variations and mutations linked to increased risk of scleroderma | Exposure to chemicals, toxins, or infections that can interact with genetic predispositions |
By understanding the complex interplay of these factors, researchers and healthcare professionals can develop more targeted and effective strategies for autoimmune disease reversal and scleroderma treatment. This knowledge is crucial in the ongoing quest to improve outcomes and enhance the quality of life for individuals affected by this challenging condition.
Diagnosing Scleroderma
Recognizing scleroderma symptoms and undergoing proper diagnostic tests are crucial steps in managing this complex autoimmune condition. Early detection can significantly improve treatment outcomes and potentially reverse the progression of scleroderma.
Symptoms Recognition
The hallmark symptom of scleroderma is the hardening and tightening of the skin, which can spread from the fingers and hands to other parts of the body. However, scleroderma can manifest in various ways, and healthcare professionals must be vigilant in identifying a range of symptoms, including:
- Raynaud’s phenomenon (abnormal blood vessel constriction)
- Digestive issues, such as difficulty swallowing or heartburn
- Lung and kidney problems
- Joint and muscle pain
Tests and Procedures
To confirm a scleroderma diagnosis, healthcare providers may order a series of tests and procedures, including:
- Physical examination: Assessing skin changes, joint mobility, and other physical symptoms
- Blood tests: Checking for specific autoantibodies associated with scleroderma
- Imaging tests: X-rays, CT scans, or MRIs to evaluate internal organ involvement
- Skin biopsy: Removing a small sample of skin for analysis under a microscope
Importance of Early Diagnosis
Early diagnosis of scleroderma is crucial for managing the condition and potentially reversing its effects. With prompt treatment, healthcare providers can address the underlying immune system dysfunction and prevent or slow down the progression of organ damage. By working closely with their healthcare team, individuals with scleroderma can develop personalized treatment plans to manage scleroderma and improve their quality of life.
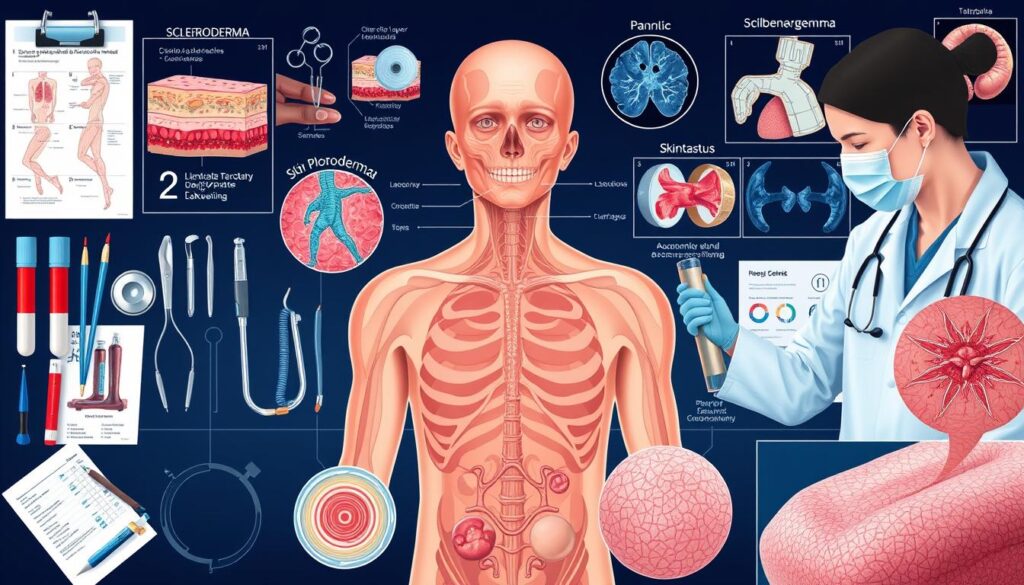
Treatment Options: A Comprehensive Guide
Living with scleroderma can be challenging, but there are various treatment options available to manage the condition and potentially reverse its progression. From conventional medical therapies to lifestyle modifications, this comprehensive guide explores the different approaches that can help individuals with scleroderma achieve better health outcomes.
Conventional Treatment Methods
Conventional scleroderma treatment often involves a combination of medications and therapies tailored to the individual’s specific symptoms and disease subtype. These may include:
- Immunosuppressant drugs to regulate the overactive immune system
- Vasodilators to improve blood flow and reduce skin tightness
- Physical therapy and occupational therapy to maintain mobility and flexibility
- Topical creams and ointments to hydrate and soften the skin
Role of Medications
Medications play a crucial role in the management of scleroderma. Depending on the individual’s condition, healthcare providers may prescribe a range of medications, including:
- Corticosteroids to reduce inflammation
- Biologics to target specific immune system components
- Antifibrinolytics to prevent the buildup of scar tissue
- Anticoagulants to improve blood flow and prevent complications
Lifestyle Modifications
In addition to medical treatments, lifestyle changes can have a significant impact on scleroderma management. Recommended lifestyle modifications include:
- Incorporating a balanced, anti-inflammatory diet rich in fruits, vegetables, and whole grains
- Engaging in regular, low-impact exercise to maintain mobility and muscle strength
- Practicing stress-reducing techniques, such as meditation or yoga, to manage emotional well-being
- Avoiding exposure to environmental triggers, such as extreme temperatures or certain chemicals
By combining conventional treatment methods, medication management, and lifestyle modifications, individuals with scleroderma can take a comprehensive approach to managing their condition and potentially reversing its effects.
| Treatment Approach | Description | Potential Benefits |
|---|---|---|
| Conventional Treatments | Medications, therapies, and procedures tailored to individual needs | Reduce inflammation, improve blood flow, and maintain mobility |
| Lifestyle Modifications | Dietary changes, exercise, and stress management techniques | Enhance overall well-being, reduce symptom severity, and potentially reverse disease progression |
Can Scleroderma Be Reversed?
While scleroderma is a challenging autoimmune disease, recent research has revealed promising insights into the possibility of reversing its effects. Experts are exploring innovative treatment approaches that aim to address the underlying causes of scleroderma, offering hope for those seeking to manage or even overcome this condition.
Current Research Findings
Researchers have been investigating various strategies to potentially reverse the progression of scleroderma. One area of focus is the role of stem cell therapy, which aims to regenerate damaged tissues and modulate the immune system. Early studies have shown that stem cell transplants may lead to significant improvements in skin thickening and organ function in some scleroderma patients.
Another promising avenue of research involves the use of targeted medications that can inhibit the signaling pathways responsible for the overproduction of collagen, a key contributor to the characteristic skin and organ fibrosis seen in scleroderma. These treatments, known as antifibrotic agents, are currently being evaluated in clinical trials to assess their ability to reverse or halt the progression of the disease.
Testimonials and Case Studies
While the road to reversing scleroderma is still under exploration, some individuals have reported remarkable improvements in their condition through a combination of conventional treatments, lifestyle changes, and alternative therapies. These case studies offer a glimmer of hope and inspiration for those living with scleroderma.
One such example is Emily, a 32-year-old woman who was diagnosed with scleroderma at the age of 28. After struggling with the debilitating symptoms for several years, Emily decided to take a holistic approach, incorporating dietary modifications, regular exercise, and stress management techniques. Over time, she noticed a significant reduction in her skin tightness, joint pain, and gastrointestinal issues, and her healthcare team observed a marked improvement in her overall condition.
While individual experiences may vary, these testimonials underscore the importance of exploring various treatment avenues and remaining hopeful in the face of scleroderma. As research continues to evolve, the possibility of reversing or even curing this autoimmune disease becomes increasingly within reach.

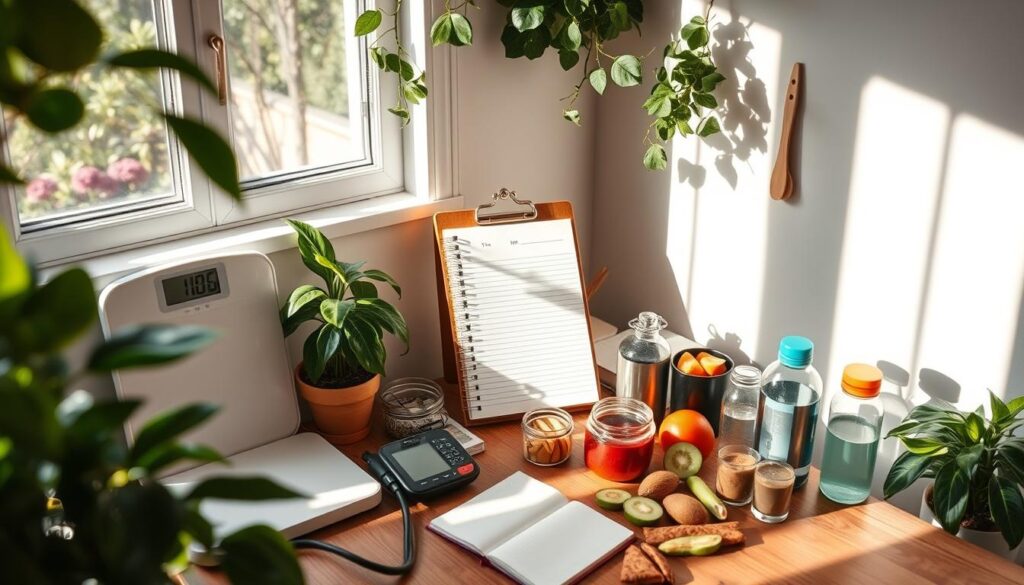
Diet and Nutrition for Scleroderma
For individuals living with scleroderma, a carefully curated diet can play a crucial role in managing symptoms and potentially reversing the condition’s progression. By focusing on anti-inflammatory foods, nutritional supplements, and avoiding certain dietary triggers, scleroderma patients can take an active approach to their well-being.
Anti-Inflammatory Foods
Incorporating anti-inflammatory foods into your scleroderma diet can help reduce inflammation and alleviate symptoms. Some of the best choices include:
- Fatty fish like salmon, mackerel, and sardines, which are rich in omega-3 fatty acids
- Leafy greens such as spinach, kale, and arugula, packed with antioxidants
- Turmeric, known for its powerful anti-inflammatory compound, curcumin
- Berries, including blueberries, raspberries, and strawberries, which are high in flavonoids
- Nuts and seeds, such as walnuts and chia seeds, providing healthy fats and fiber
Nutritional Supplements
In addition to a nutrient-dense diet, certain supplements may offer additional benefits for individuals with scleroderma. These may include:
- Vitamin D, which plays a role in immune function and can help manage autoimmune conditions
- Probiotics, to support gut health and reduce inflammation
- Antioxidants like CoQ10 and N-acetylcysteine, which can help protect against oxidative stress
- Herbs such as ginger and boswellia, known for their anti-inflammatory properties
Foods to Avoid
While incorporating beneficial foods is essential, it’s equally important to identify and limit or eliminate any dietary triggers that may exacerbate scleroderma symptoms. These may include:
- Processed and fried foods, high in unhealthy fats and additives
- Refined carbohydrates, such as white bread and pastries
- Alcohol, which can contribute to inflammation
- Dairy products, which may trigger an immune response in some individuals
By making informed choices about your scleroderma diet and incorporating natural remedies, you can take a proactive approach to managing this complex condition and potentially improve your overall well-being.
Physical Therapy and Exercise
Scleroderma, an autoimmune condition that affects the connective tissue, can significantly impact an individual’s physical abilities. However, regular exercise and physical therapy can play a vital role in managing the symptoms and improving overall quality of life for those living with scleroderma.
Benefits of Regular Exercise
Engaging in physical activity can provide numerous benefits for individuals with scleroderma, including:
- Improved joint mobility and flexibility
- Increased muscle strength and endurance
- Enhanced cardiovascular health
- Reduced fatigue and improved energy levels
- Better circulation and skin health
Recommended Exercises
When it comes to scleroderma management, not all exercises are created equal. Here are some recommended exercises that can be particularly beneficial:
- Low-impact aerobic activities, such as walking, swimming, or cycling
- Gentle stretching and range-of-motion exercises
- Strength training with light weights or resistance bands
- Tai chi or yoga, which can improve balance and flexibility
Finding a Therapist
Working with a physical therapist who specializes in autoimmune conditions like scleroderma can be invaluable. These professionals can create personalized exercise programs, provide guidance on managing symptoms, and offer support throughout the journey. When searching for a suitable therapist, look for one with experience in scleroderma management and a holistic approach to patient care.
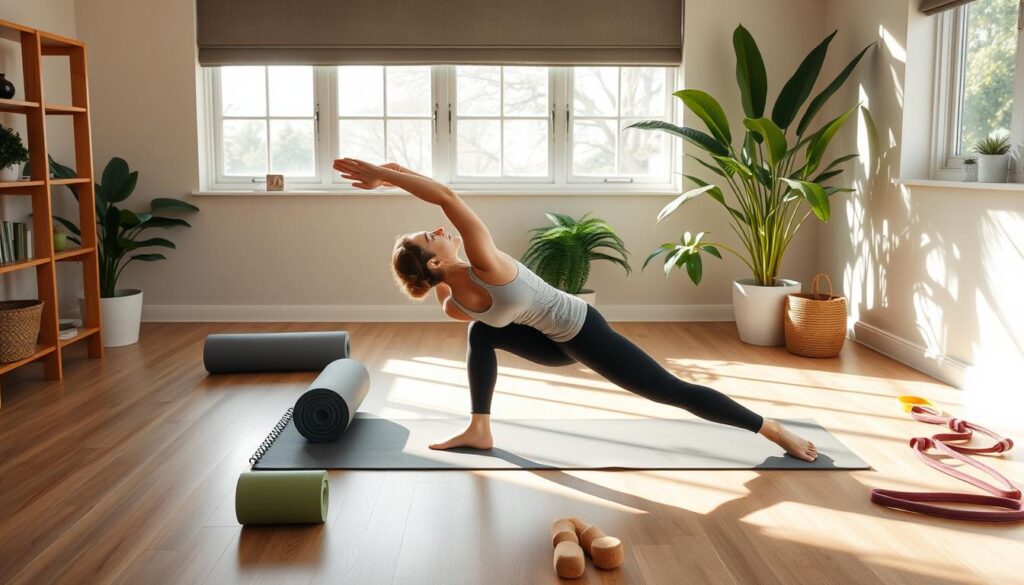
By incorporating regular physical therapy and exercise into their scleroderma management plan, individuals can take an active role in improving their physical and overall well-being. Whether it’s improving joint mobility, increasing strength, or enhancing cardiovascular health, these lifestyle changes can make a significant difference in the lives of those living with scleroderma.
Alternative Therapies and Approaches
For individuals living with scleroderma, seeking relief beyond traditional medical treatments can be a meaningful part of their journey. While conventional therapies are crucial, alternative therapies and approaches may offer additional benefits in managing symptoms and improving overall well-being. Let’s explore some of these complementary options that are gaining traction in the scleroderma community.
Acupuncture and Its Benefits
Acupuncture, a traditional Chinese practice, has shown promise in providing relief for scleroderma patients. By targeting specific meridian points in the body, acupuncture is believed to restore balance and promote the flow of vital energy, or qi. Studies have suggested that acupuncture can help alleviate symptoms such as Raynaud’s phenomenon, skin tightness, and joint pain associated with scleroderma.
Herbal Remedies
The use of herbal remedies, a cornerstone of natural remedies for scleroderma, has gained attention among scleroderma patients. Certain herbs, such as cat’s claw, ginkgo biloba, and green tea, have demonstrated anti-inflammatory properties that may help manage the underlying immune system dysfunction in scleroderma. Always consult with a healthcare provider before incorporating scleroderma alternative medicine into your treatment plan.
Mindfulness and Stress Management
Stress can have a significant impact on the progression and management of scleroderma. Incorporating mindfulness practices, such as meditation, deep breathing, and yoga, can help individuals with scleroderma better manage stress and anxiety. These techniques have been shown to reduce inflammation, improve sleep quality, and enhance overall well-being.
By exploring these alternative therapies and approaches, individuals with scleroderma can take an active role in their healthcare and potentially find additional ways to alleviate their symptoms and improve their quality of life. As always, it is essential to work closely with a healthcare team to ensure a comprehensive and well-rounded treatment plan.

Living with Scleroderma
Navigating life with scleroderma can be a daunting experience, but with the right coping mechanisms and support, patients can learn to manage the condition effectively. Scleroderma management is crucial for maintaining a good quality of life, and scleroderma lifestyle changes can make a significant difference in managing the symptoms and progression of the disease.
Coping Mechanisms
Dealing with the physical and emotional challenges of scleroderma requires a multi-faceted approach. Some effective coping mechanisms include:
- Adopting stress-reduction techniques, such as meditation, yoga, or deep breathing exercises, to help manage anxiety and depression.
- Seeking counseling or joining support groups to connect with others who understand the unique experiences of living with scleroderma.
- Maintaining a positive outlook and practicing self-care, such as getting enough rest, eating a healthy diet, and engaging in gentle exercise.
Support Groups and Resources
Connecting with others who share your experiences can be incredibly beneficial for scleroderma patients. Support groups, both in-person and online, provide a safe space to share stories, receive emotional support, and learn from one another’s experiences. Additionally, there are numerous resources available, such as educational materials, advocacy organizations, and assistance programs, that can help individuals with scleroderma navigate their condition and access the support they need.
| Resource | Description |
|---|---|
| Scleroderma Foundation | A leading non-profit organization that provides education, support, and research for individuals with scleroderma. |
| Scleroderma Research Foundation | A dedicated research organization focused on finding a cure and better treatments for scleroderma. |
| Scleroderma Support Groups | Local and online support groups that offer a community for individuals living with scleroderma. |
By embracing scleroderma management strategies and accessing the available resources, individuals with scleroderma can learn to navigate their condition and improve their overall well-being.

Monitoring Progress: Keeping Track
Scleroderma is a complex and chronic condition that requires diligent management and ongoing monitoring. Regular check-ups with your healthcare team are essential to ensure the effectiveness of your treatment plan and to identify any changes or new developments in your condition.
Importance of Regular Check-Ups
Routine medical appointments allow your doctor to assess your overall health, monitor the progression of scleroderma, and make any necessary adjustments to your treatment. These check-ups may include physical examinations, diagnostic tests, and discussions about your symptoms, concerns, and treatment goals.
Tracking Symptoms and Treatments
- Keep a detailed record of your scleroderma symptoms, including their severity, frequency, and any changes over time.
- Document the medications, therapies, and lifestyle modifications you are currently using to manage your condition.
- Note any side effects or changes in your response to various treatments.
Adjusting Treatment Plans
Based on the information gathered during your regular check-ups and your symptom tracking, your healthcare team can work with you to fine-tune your treatment plan. This may involve adjusting medication dosages, trying new therapies, or exploring alternative approaches to better manage your scleroderma.
| Symptom | Severity | Treatment | Response |
|---|---|---|---|
| Skin tightening | Moderate | Topical corticosteroids | Improved significantly |
| Raynaud’s phenomenon | Severe | Calcium channel blockers | Moderate improvement |
| Fatigue | High | Lifestyle modifications, exercise | Noticeable reduction |
Staying actively involved in your scleroderma management and working closely with your healthcare team is key to achieving the best possible outcomes and potentially reversing the progression of this challenging condition.
Future Directions in Scleroderma Research
As researchers delve deeper into the complexities of scleroderma, a glimmer of hope has emerged for those living with this challenging condition. The field of scleroderma research is rapidly evolving, with scientists exploring cutting-edge therapies and innovative approaches that may hold the key to reversing the effects of this autoimmune disorder.
Breakthroughs in Treatment
One of the most promising areas of scleroderma research is the development of stem cell therapy for scleroderma. Scientists are investigating the use of stem cells to regenerate damaged tissues and organs, offering the potential to reverse the progressive nature of scleroderma. Early clinical trials have shown encouraging results, with some patients experiencing improved skin and organ function after undergoing stem cell transplants.
Ongoing Clinical Trials
- Researchers are currently exploring the use of targeted immunotherapies to modulate the overactive immune system, which is a key driver of scleroderma.
- Clinical trials are also examining the efficacy of novel antifibrotic medications, aimed at halting the excessive scarring that is a hallmark of scleroderma.
- Innovative approaches, such as gene therapy and cell-based therapies, are in various stages of development, providing hope for a scleroderma cure in the future.
Hope for New Therapies
As the scientific community continues to make strides in understanding the underlying mechanisms of scleroderma, the future holds promising possibilities for those affected by this condition. With ongoing research and clinical trials, the potential for new and effective treatments is steadily growing, offering hope for a brighter tomorrow for individuals living with scleroderma.
“The future of scleroderma treatment is filled with excitement and optimism. We are on the cusp of breakthrough discoveries that may transform the lives of those living with this debilitating condition.”
– Dr. Emily Harrington, leading scleroderma researcher
| Innovative Therapies | Potential Benefits |
|---|---|
| Stem Cell Therapy | Regeneration of damaged tissues and organs |
| Targeted Immunotherapies | Modulation of the overactive immune system |
| Antifibrotic Medications | Halting of excessive scarring |
| Gene Therapy and Cell-based Therapies | Addressing the root causes of scleroderma |
Seeking Professional Help
If you suspect you may have scleroderma or are experiencing persistent symptoms, it’s crucial to seek professional medical assistance. Consulting a specialist, such as a rheumatologist or dermatologist, can provide you with the proper diagnosis and ensure you receive the most appropriate treatment plan to manage your condition.
When to Consult a Specialist
You should consider seeing a scleroderma specialist if you notice any of the following: persistent skin tightening or hardening, joint pain, digestive issues, or difficulties with breathing or circulation. These symptoms may indicate the presence of scleroderma, and early intervention is essential for effective management and potentially reversing the condition.
Finding the Right Healthcare Team
Assembling a team of healthcare professionals who specialize in scleroderma is crucial for your well-being. This team may include a rheumatologist, dermatologist, physical therapist, and other specialists, depending on your specific needs. Work closely with your doctors to develop a comprehensive treatment plan that addresses all aspects of your condition.
Questions to Ask Your Doctor
When meeting with your healthcare providers, be prepared to ask questions about your scleroderma diagnosis, treatment options, and the potential for reversing the condition. Some important questions to consider include: What stage of scleroderma do I have? What are the best treatment approaches for my specific case? Are there any clinical trials or new therapies I should be aware of? How can I monitor my progress and adjust my treatment plan as needed?